How AI and Implementation Science Could Bridge the Mental Health Access Gap
With over 160 million Americans living in mental health professional shortage areas, the U.S. continues to face a worsening behavioral health access crisis. This challenge is especially acute in Medicaid-reliant and underserved regions, where clinics often struggle to recruit and retain licensed providers. For federal policymakers and state systems, the question is no longer whether reform is needed, but how to scale solutions that work.
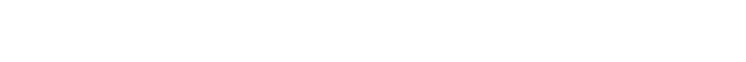
Dr. Yuanyuan Hu, Assistant Professor at the University of Minnesota School of Social Work, is proposing one such solution—one that brings together integrated behavioral health, implementation science, and community-based mental health workforce development. Her research aims to equip paraprofessionals (peer specialists, case managers, community health workers, etc) with real-time, adaptive AI support tools that allow them to support mental health care delivery in their communities in conjunction with traditional treatment systems.
Her work is grounded in a strong scholarly foundation, has already been cited in influential scholarship, and has received institutional backing—all of which shows significant promise to the U.S. healthcare and public service sectors.
Foundation in Integrated Behavioral Health Care
Dr. Hu’s proposal builds on her previous research evaluating Certified Community Behavioral Health Clinics (CCBHCs)—federally supported demonstration programs designed to expand access to mental health and substance use treatment, and an integrated clinic and service delivery model that provides a comprehensive range of mental health and substance use services. Her 2021 publication on the topic, co-authored with researchers at NYU, has been cited by scholars in leading behavioral health journals. Dr. David Hodgkin, a behavioral health economist, whose own federally supported work cited Dr. Hu’s findings. “The model is inspired by studies of co-occurring mental health and substance use disorders, which recommended integrating specialty behavioral health treatment and coordinating with primary care to address both disorders.”
Proposed Use of AI to Expand the Workforce
At the core of Dr. Hu’s approach is the use of advanced NLP algorithms to evaluate clinic notes for person-centered principles and identify effective care coordination patterns from EHR data in integrated behavioral health clinics. Dr. Hu is leading the creation of high-quality, culturally responsive datasets to fine-tune LLMs for community-based organizations. By offering AI-based instruction on psychoeducation, early symptom detection, and referral to formal treatment, this project tackles workforce deficits head-on, laying cost-effective pathways to quality behavioral health treatment and fueling the nationwide expansion of integrated behavioral health care. These findings inform the design of LLM-powered training platforms and tools, ensuring that best practices derived from real-world data are embedded into scalable, evidence-based interventions. This approach strengthens the national behavioral health infrastructure by enabling more targeted, culturally responsive, and cost-effective services.
Once implemented, the platform has the potential to improve paraprofessional retention, strengthen care coordination, and reduce documentation burdens—key operational barriers in Medicaid-funded and integrated care settings.
Recognition from Academic and Policy Institutions
Dr. Hu’s work has been published in high-impact journals such as Psychiatric Services, The Journal of Behavioral Health Services & Research, and JMIR Medical Informatics. Her research has been cited in top-tier, peer-reviewed behavioral health journals. Further, Dr. Hu received a grant from the C.V. Starr Fund for Asian/Pacific/American Research—administered by the Asian/Pacific/American Institute at NYU—to support her doctoral research on behavioral health integration for older Chinese immigrants. The grant supports academic projects with applied policy value and is awarded to research that bridges theory and real-world practice.
“That grant-funded work that continues to influence my models today,” Dr. Hu said.
“It helped clarify how community-based, culturally tailored care can be systematized—not just theorized.”
Tapping Into National Health Priorities
Dr. Hu’s research doesn’t exist in isolation—it closely mirrors the direction of several major federal health initiatives. Her focus on AI-supported training for paraprofessionals and equitable behavioral health delivery is directly aligned with the Substance Abuse and Mental Health Services Administration (SAMHSA)’s 2023–2026 Strategic Plan, which advocates for expanding the behavioral health workforce through peer support models and culturally competent care.
Her work also reflects the goals of the U.S. Department of Health and Human Services’ Equity Action Plan, which prioritizes scalable, community-based infrastructure to reduce disparities in underserved populations. Similarly, her research approach echoes priorities laid out in the National Institutes of Health’s 2024–2029 Strategic Framework, which calls for technology-driven, implementation-ready innovations to improve access to behavioral health services nationwide.
Conclusion: A Research-Based Endeavor with National Implications
Dr. Hu’s work is a research-driven endeavor that addresses critical gaps in the U.S. behavioral health system through the development of AI-enabled training platforms for paraprofessionals. The value of Dr. Hu’s contribution lies in her ability to generate original, policy-relevant research that informs how mental health services may be improved, particularly in underserved communities. Her studies are not speculative—they are backed by competitive grants, published in respected journals, and cited by scholars and policy analysts focused on national systems reform.
Dr. Hu’s research stands on its own as a nationally important effort and provides a strong foundation for future solutions in healthcare access and workforce development across the United States.
Nia Caldwell is a health equity writer and editorial researcher with a social work and public interest journalism background. She specializes in profiling individuals and initiatives reshaping care from the ground up. Based in Chicago, Nia divides her time between community-centered storytelling and reporting on innovation in behavioral health.