Inflammation’s Silent Conductors: How Dr. Rahmeh Othman’s Insights Into Kinins and Receptor Signaling Are Revolutionizing Retinal Inflammation Therapies
In the quiet, light-sensing world of the retina, microscopic molecular conversations decide whether vision endures or fades. For millions with diabetic retinopathy, that communication has long been in chaos—interpreting healing messages into burning inflammation that steals vision cell by cell.
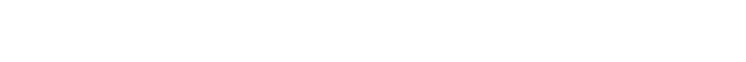
The code breaker behind this undercover score is Dr. Rahmeh ‘Ro’ Othman, a highly sought-after postdoctoral fellow in immunology at Harvard Medical School whose seminal research on receptor signaling has established her as the go-to scientist in retinal inflammation studies.
She says: “What drew me to this field of research was curiosity—the need to understand why some inflammatory pathways fail and how they could be redirected. I wanted not only to identify the molecules at fault but to find ways to translate those findings into practical treatments. Learning which components lead the inflammatory ‘orchestra’ lets us retune it rather than silence it.”
For decades, treatment meant injections deep into the eye or complex surgeries that often failed a third of patients. Yet today, a different melody is emerging—one carried by the microscopic “conductors” of inflammation known as kinins. While many studies of diabetic eye disease center on vascular damage, Dr. Othman’s work focuses on the molecular signaling that triggers inflammation long before visible tissue changes appear.
Her work reveals how these elusive peptides and their receptors orchestrate inflammation in ways traditional therapies have overlooked. By mapping how kinin receptors misfire inside diseased retinas, Dr. Othman shows that vision loss may one day be prevented not with needles, but with a few drops of targeted medicine.
Her curiosity for molecular meaning soon evolved into a guiding principle: bridge every mechanism to a tangible outcome patients can feel.
Bridging Mechanism and Meaning
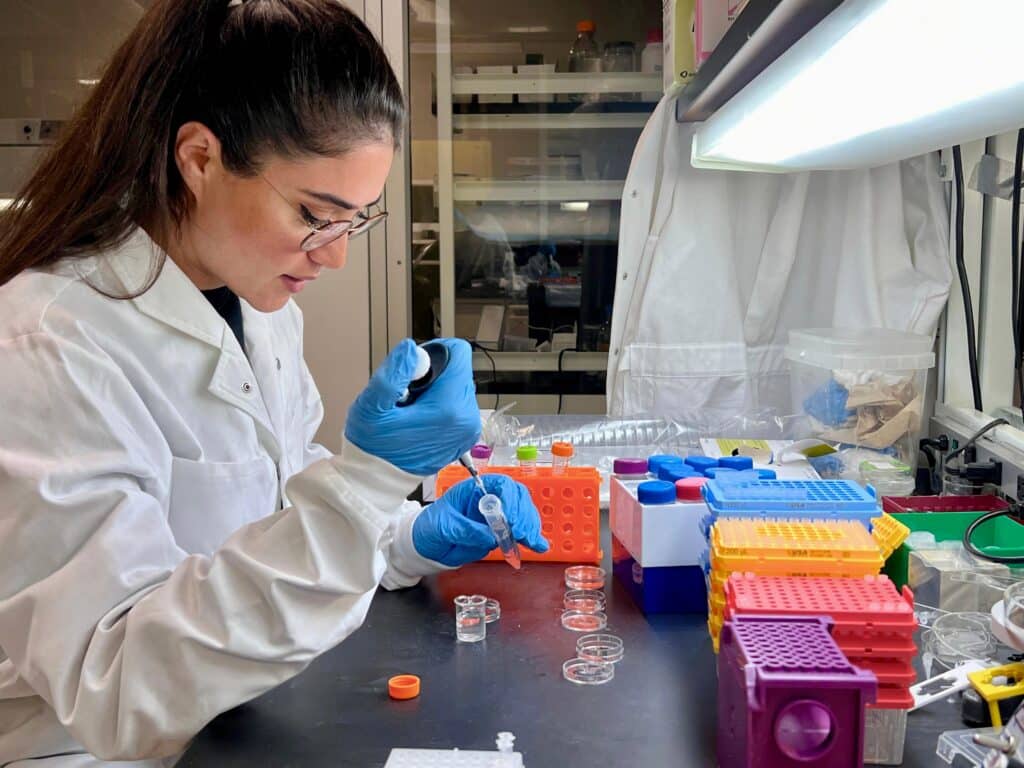
Long before her current postdoctoral work, Dr. Othman built a decade of translational research across immunology, neurobiology, molecular biology and physiology—moving fluid findings into clinically minded designs. From in-vivo models to biomarker panels and optimized assays, she consistently converts molecular observations into actionable therapeutic hypotheses.
Dr. Othman says: “When I joined research, I realized that discovery isn’t enough—our real calling is taking knowledge and creating impact. Every assay, every model, is a language that helps patients be heard in molecular terms. That’s why I demand that data be connected to outcomes; otherwise, knowledge remains locked in the lab.”
That conviction — science in service of people — underpins her approach: rigorous, systematic, and always translational. It’s this balance between precision and purpose that defines her philosophy—anchoring her belief that science itself is a systemic dialogue between data and healing.
Her guiding principle met its first true test in the study of kinins—tiny peptides whose miscommunication can ignite inflammation, turning repair into destruction.
Decoding the Kinins: Rewriting Inflammation Biology
Kinins may not be familiar to patients, but in the field of inflammation, they are fast becoming headline molecules. They act as signal carriers, binding to receptors bradykinin type 1 (B1R) and type 2 (B2R) that can either calm or inflame tissue. Dr. Othman’s work reframed these receptors as key decision-makers in retinal disease.
Her doctoral dissertation first identified the B1R receptor’s role in diabetic retinal inflammation, producing pre-clinical evidence that modulating this receptor could mitigate vascular leakage and oxidative stress.
She explains: “During my Ph.D., I uncovered that the B1R receptor–inducible nitric oxide (iNOS) axis plays a key role in triggering inflammation in diabetic retinopathy. Blocking that axis early on actually reversed the inflammation, which was a striking result. What made it even more meaningful was confirming the receptor’s presence in human retinal tissue, proving that the findings could translate into real treatments—simple, accessible, and potentially as easy as using eye drops.”
These findings are based on a well-designed experiment. Assays such as ELISA, qPCR, RNAScope, and high-resolution microscopy will enable her team to chart molecular pathways with precision and translate incoherent receptor behavior into tangible therapeutic targets.
She reflects: “For years, kinins were treated like background noise in the inflammation symphony. But once we started isolating their patterns, the melody became clear—they’re not just messengers, they’re conductors. Understanding that changed how we design therapies, because now we’re targeting the rhythm, not just the notes.”
Her 2019 article in Frontiers in Pharmacology, which identified the B1R receptor-iNOS axis as a driver of diabetic retinopathy, has become a widely cited point of reference in treatment. Subsequent research in Cells and Pharmaceuticals documented receptor expression in the human retina and proposed non-invasive treatments, firmly locating her among the scientists shaping contemporary ocular pharmacology.
Professor Réjean Couture, former Director of the Post-Graduation Program in Physiology at the Université de Montréal, notes that her discoveries helped define new departmental standards for ocular-inflammation research: “Dr. Othman was instrumental in creating our ocular-inflammation research framework, developing the protocols and analytical standards that remain integral to our retinal pharmacology studies today.”
He adds that her methods: “are now reference points across our department, guiding everything from retinal permeability assays to therapeutic screening.”
Dr. Othman’s work represents lasting institutional influence, with this emerging scientist continuing to shape how ocular-inflammation studies are conducted across North America. Since then, many laboratories have adopted her experimental pipelines—a testament to the broader impact and influence she has had through her research in the field.
The same logic that clarified the retina soon expanded into a system-wide investigation of inflammation itself, revealing that molecular signaling is part of a continuous scientific conversation—a systemic dialogue linking the eye, gut, and brain.
Beyond the Eye: System-Wide Insights into Inflammation
That integrative mindset culminated in her 2025 publication she contributed to in “Cell, Enteric neuronal mechanosensation by Piezo1 orchestrates intestinal motility and mucosal inflammation.” With Cell’s impact factor exceeding 45, the study represents the pinnacle of scientific rigor.
Dr. Othman’s co-authorship signified contributions that met the journal’s highest standards, validating her experimental mastery in the gut’s neural–immune landscape.
Dr. Othman says: “What fascinated me most was realizing that inflammation doesn’t respect borders. The same mechanisms that inflame a retina can disrupt the gut or the brain. Once you grasp that unity, it’s impossible to study one organ in isolation—you start thinking in networks, not tissues.”
Her investigations into neuro-immune interplay reveal striking parallels: while distinct receptors modulate retinal inflammation, pain, and gut disorders such as inflammatory bowel disease (IBD), her work highlights converging pathways through which immune and neuronal signals intersect across these systems. This interconnected web—evident in her preclinical models of enteric neuron function and biomarker analyses of immune responses—underscores how inflammation weaves together distant physiological domains.
Using an optogenetic platform to manipulate the activity of the neurons, Dr. Othman explains: “Wireless optogenetics allows us to listen in on the body’s private conversations—it lets us observe how nerves and immune cells interact in real time. This level of precision doesn’t just shed light on gut physiology; it helps decode the broader language of inflammation, from the retina to the intestines.’’
These findings were furthered by earlier reviews in the Journal of Internal Medicine in 2019 and the Journal of Allergy and Clinical Immunology in 2024, establishing one of the first integrative models for combined neuro-immune signaling. These, when combined, position Dr. Othman at the forefront of cross-system inflammation research.
Building on this foundation, her current preclinical research at Harvard explores neuro-immune interactions within the gastrointestinal tract. It seeks to identify therapeutic targets that could redefine the treatment of IBD. By applying wireless optogenetics in freely moving animal models, she achieves a new level of precision in mapping how neuronal activity shapes immune responses in real time.
She says: “Each field I’ve worked in—ocular, gastrointestinal, respiratory—taught me something about how the body communicates with itself. The techniques we use, from in vivo neural implants to molecular imaging, let us study that dialogue on terms we could never reach before.”
Her integrated approach, which utilizes imaging, molecular characterization, and functional modeling, views inflammation as a systemic dialogue rather than a regional flaw, distilling decades of expertise into a cohesive framework. These investigations demonstrate how her methodological breadth continues to drive discovery across organ systems.
This work repositions inflammation not as an isolated dysfunction, but as an ongoing biological dialogue; it illustrates inflammation as a site and medium of such a dialogue in the entirety of the organs.
Peer Review and Collaborative Scholarship
Dr. Othman is recognized for her integrity, scientific rigor, and critical insight—qualities that have earned her respect within the international research community. She serves as a regular peer reviewer for several high-impact, MDPI-indexed journals, including the Journal of Clinical Medicine (clinical and translational research), Tomography (medical imaging), and Pharmaceuticals (drug discovery and pharmacology). Her thorough and discerning reviews have shaped the publication landscape in fields spanning immunophysiology and inflammation biology.
She reflects: “Peer review is an invisible service. You lend your time so that the science reaching the public stands on solid ground. I see it as both a duty and a dialogue—every review teaches me something new about clarity, rigor, or humility.” It’s an insight that mirrors her collaborative style in the lab.
A specific significance of Dr. Othman’s contribution lies in how her systemic view of inflammation—treating it as a body-wide conversation rather than a localized defect—has reshaped how teams design retinal disease models and interpret neuro-immune data. Her collaborations and invited reviews amplify that influence, helping set methodological standards that other groups adopt.
In doing so, she strengthens the scientific dialogue itself—making exchanges of knowledge more transparent, interconnected, and reliably actionable.
Shaping a New Therapeutic Horizon
The potential of Dr. Othman’s discoveries extends far beyond academia. Diabetes-related retinal diseases burden health systems with billions of dollars in costs annually, and many patients remain inadequately treated..
Her work provides strong evidence that kinin-targeted eye drops could dramatically reduce both cost and patient risk, potentially shifting the standard of care from invasive procedures to accessible, non-invasive therapy.
She explains: “Finding these inflammatory pathways gives us a blueprint for far more than one disease. The same molecular circuits appear in diabetes, intestinal disease, and even chronic pain — and connecting those hidden links shows how inflammation behaves as a single system.”
Through several peer-reviewed publications and invited chapters—from Pediatric Research to Cell—Dr. Othman illustrates how mechanistic insights at the molecular level can be translated into therapies with a global impact. She actively disseminates these findings through international conference presentations and rigorous peer-review service, helping to set standards and advance the field of inflammation biology.
She says: “Every dataset traces back to a patient. Someone’s parent, someone’s child, is waiting for the next therapy. Even the smallest finding matters — it shifts the future for people we may never meet.”
At Harvard Medical School, Dr. Othman continues to explore how immune and neural systems converge across organs — from the gut to the eye — to translate complex interactions into safe, home-ready therapies.
She adds: “I hope future scientists keep linking molecular insight to patient outcomes. Discovery should always stay anchored in public health impact, because every step in science is a step toward easing someone’s suffering.”
Dr. Othman’s distinct vantage point, with its foundation in both scientific rigor and human compassion, remains one of the most trusted voices in this area of inquiry today. Inflammation biology doesn’t look like a disorder anymore, it seems like a dance—an emotive exchange of choreography where we can match precision with compassion.