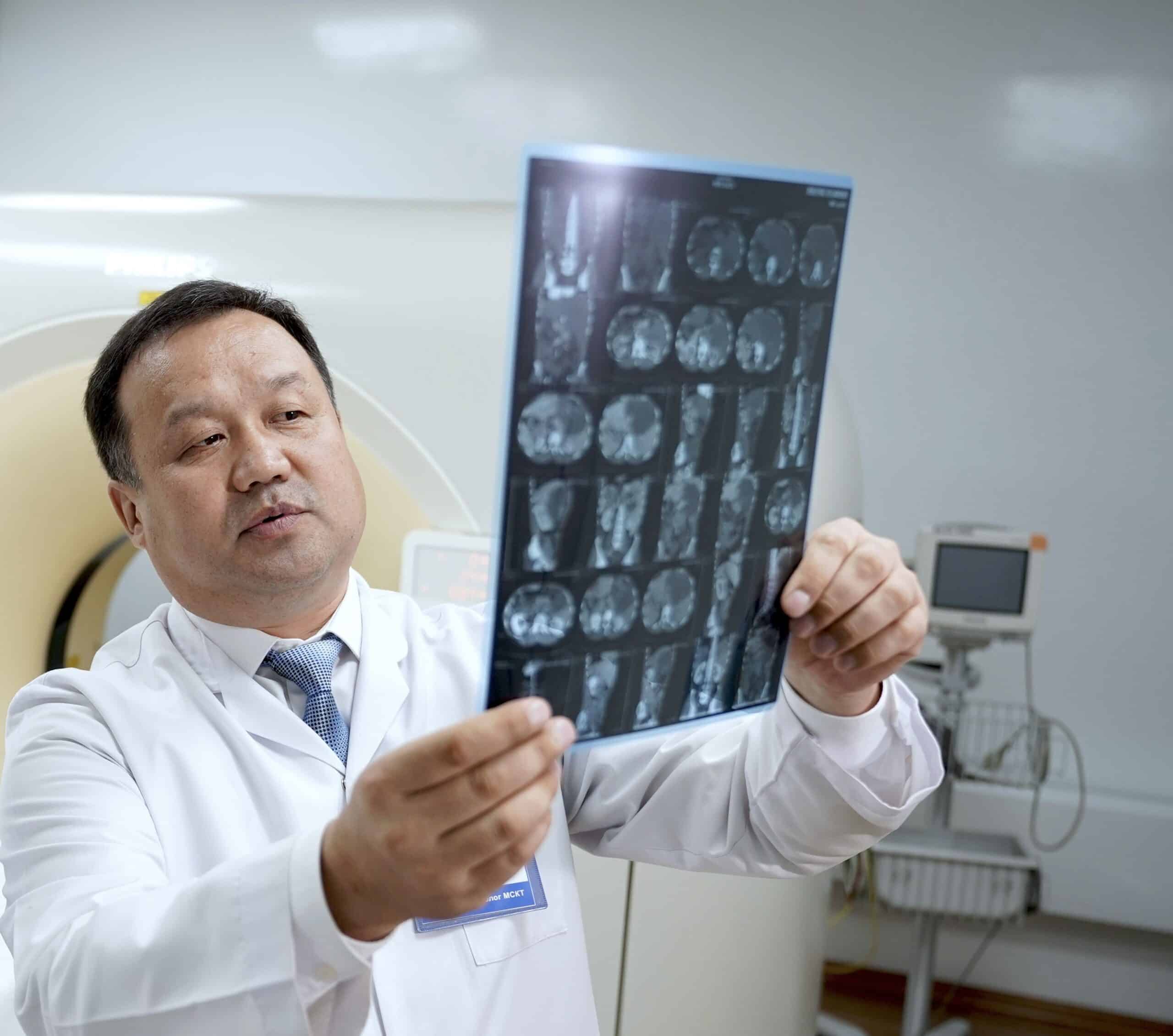
Zhyrgalbek Zhakypov: The Radiologist’s Task is to Provide a Complete Picture for Choosing the Optimal Treatment Strategy
Diagnostic imaging is one of the key tools of modern medicine, which relies on preventive strategies. This is confirmed by data from the European Society of Radiology (ESR) and the World Economic Forum, according to which up to 80–90% of all key clinical decisions today are made based on medical imaging. Against the backdrop of global efforts to combat dangerous pathologies such as breast cancer, specialists who combine fundamental clinical experience with mastery of high-tech visualization methods are coming to the forefront. One such specialist is Zhyrgalbek Zhakypov—an expert physician at a major international diagnostic center in Bishkek and member of the Association of Radiologists of the Kyrgyz Republic. A specialist with 23 years of experience who has progressed from military field doctor to expert in modern imaging methods, Zhyrgalbek Zhakypov spoke with us about the technological breakthrough in Kyrgyz radiology, modern visualization methods, and his participation as a judge for the “Best Talents” award.
– Statistics indicate that up to 90% of clinical decisions today are based on information from medical imaging. Do you agree with these figures?
– Yes, these statistics reflect the massive changes I’ve observed throughout my career. If 23 years ago, at the start of my journey, medical imaging was considered merely supplementary, today it has become a tool without which it’s practically impossible to make an accurate diagnosis. In my practice, there have been numerous cases where an MRI or CT scan changed the treatment plan, allowing us to avoid unnecessary interventions or, conversely, detect critical pathology in time. But we must remember that an image is nothing without expert interpretation.
– Speaking of expertise, there’s a clear trend toward multidisciplinarity in diagnostic imaging—physicians with deep knowledge across different fields play a special role here. Your professional path—internist, infectious disease specialist, radiologist—fits this trend well. How does this versatility help in making error-free decisions when diagnosing complex cases?
– A radiologist needs the ability to analyze pathological processes in the context of the body’s entire physiology. I’ve worked as an internist, infectious disease specialist, and head of medical services, and all of this has shaped my clinical perspective. For example, experience in infectious diseases is critically important when differentiating inflammatory changes in the lungs, which became obvious during the pandemic, while my internal medicine background helps me interpret systemic diseases more accurately. A comprehensive approach allows me not just to state the presence of a lesion on an image, but to give the treating physician a complete picture for choosing a treatment strategy.
– You’re among Kyrgyzstan’s leading radiologists and offer your patients the widest possible range of examinations. In what cases should someone see a diagnostic imaging specialist?
– When testing is needed due to symptoms and when we want to make sure there are no problems, at the prevention stage. In the first case, this applies to any unclear conditions—from a prolonged cough to joint discomfort: when there’s clinical uncertainty, CT or MRI helps clarify the diagnosis. On the other hand, modern medicine is increasingly moving toward prevention, and here diagnostic imaging serves as the main tool for cancer screening. Many insidious diseases, including lung, colon, or breast tumors, show no symptoms in their early stages. That’s why periodic examinations, such as low-dose computed tomography or quality ultrasound, are indicated for people in risk groups. This allows us to detect disease when it’s still curable.
– Tell us about the modern radiologist’s arsenal and which pathologies make your methods a decisive factor in diagnosis.
– Today’s radiologist works at the intersection of cutting-edge engineering and fundamental medicine. At my disposal are multi-slice computed tomography scanners (MSCT) capable of creating thousands of slices of the human body in seconds, and magnetic resonance imaging scanners (MRI) that allow us to look inside soft tissues without surgical intervention. The spectrum of diseases we diagnose covers virtually all areas of medicine, but in some cases our findings carry special weight. In oncology, this means detecting tiny tumors and monitoring chemotherapy effectiveness; in cardiology, assessing coronary artery condition. We identify complex pathologies of the central nervous system, such as multiple sclerosis or early stages of Alzheimer’s disease, and diagnose acute conditions: strokes, internal bleeding, and complex injuries.
– I’m sure you pay special attention to mammography as a tool for early breast cancer detection—this is a serious problem for Kyrgyzstan. Tell us what enables you to detect pathology in its early stages.
– Indeed, the breast cancer situation in the republic is severe—60–70% of patients are diagnosed at stage 3 or 4. My colleagues and I are trying to change these statistics for the better. Of course, technical equipment helps—for instance, I work with a modern Senographe Pristina mammography system manufactured by General Electric, performing mammography with 3D tomosynthesis, which ensures high diagnostic accuracy. This technology allows the physician to see breast tissue layer by layer, without “overlapping,” so small changes and early lesions aren’t lost in the images. In the future, we plan to launch a free mammography program with 3D tomosynthesis at our center.
– You’re an active member of the Kyrgyz Association of Radiologists and a regular expert and participant at specialized conferences. What tasks do you consider priorities for yourself as a national-level expert in the coming years?
– On one hand, our field is experiencing a technological breakthrough—Bishkek and Osh have expert-class equipment, and converting several facilities to 24-hour operation while introducing social tariffs has made CT and MRI more accessible. On the other hand, regional imbalance persists: in remote areas, patients spend hours traveling to get basic scans. A serious problem is the shortage of personnel. I consider the priorities to be, first, developing teleradiology, namely implementing the Picture Archiving and Communication System (PACS), which allows images to be transmitted from the regions to Bishkek, where experts can consult patients from across the country. Second, integrating AI services to automate routine tasks and minimize the risk of human error. Finally, standardization and continuous education are critically important.
– You’re also considered an expert in such a modern diagnostic imaging method as multi-slice computed tomography. What complex pathologies requiring expert image analysis have been detected more frequently thanks to your work with MSCT?
– Thanks to MSCT, we’ve been detecting complex vascular pathologies more often, including aneurysms and thromboses in early stages, changes in lung tissue, initial manifestations of interstitial diseases, as well as combined injuries where it’s important to quickly and accurately assess multiple anatomical zones simultaneously. A separate direction is oncological cases: MSCT makes it possible to assess in detail the extent of the process and involvement of surrounding structures, which directly affects treatment strategy.
– Global radiology today is moving from descriptive reports to precise measurements of tissue parameters. Tell us about CT densitometry and CT angiography—visualization methods that achieve this.
– CT angiography allows non-invasive examination of the vascular system, detecting congenital anomalies, aneurysms, and stenoses long before critical complications occur. In oncology, this method is indispensable for assessing tumor blood supply. As for CT densitometry, it enables us to measure bone mineral density with mathematical precision. This is a fundamental tool for diagnosing osteoporosis and assessing risks of pathological fractures. Preventive imaging methods allow us to move from subjective assessments to objective digital parameters.
– Your expertise and experience allowed you to become a judge for the “Best Talents” award, where you evaluated colleagues’ achievements. You also teach medical college students and physicians working in the Ministry of Internal Affairs system. What advice do you give young colleagues striving to become international-level professionals?
– My main advice is discipline in everything: in study, in work, and in life. This is the key to success in our specialty. Second, genuine love for people: without empathy, it’s impossible to become a good doctor. And of course, continuous development is necessary: technologies in medicine change faster than textbooks. Anyone who wants to become a leader must be able to quickly assess changes in the field, be the first to implement innovations in practice, and teach this to colleagues.